A Low FODMAP Diet Chart is a helpful tool for managing digestive discomfort.
It lists foods that are low in certain carbohydrates that can trigger tummy troubles.
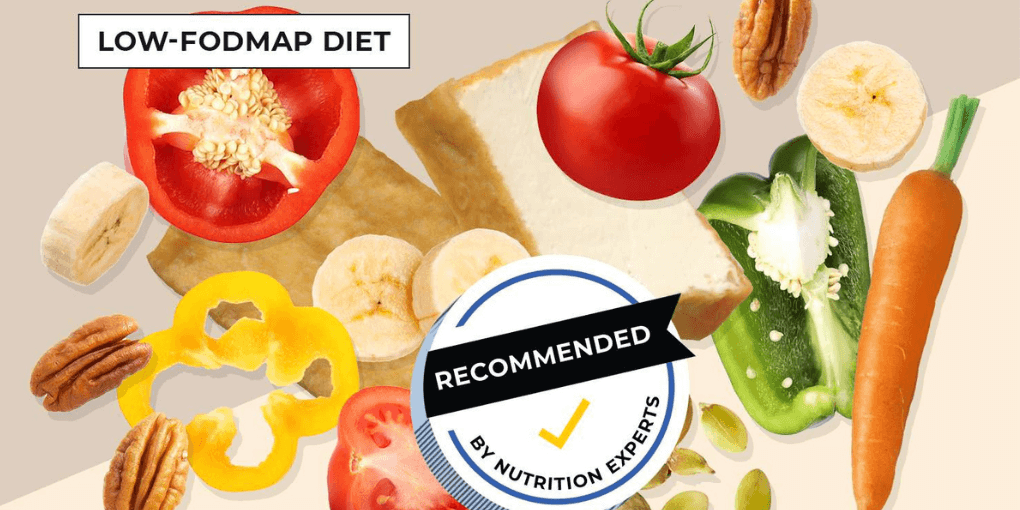
This diet is often recommended for those with irritable bowel syndrome (IBS) or other gut issues.
By following this chart, you can reduce symptoms like bloating, gas, and stomach pain.
It’s important to work with a healthcare professional or dietitian to create a personalized plan that suits your needs.
In collaboration with Nour Zibdeh, a distinguished authority in Integrative & Functional Nutrition, this blog is designed to harness our collective expertise.
With a focus on practical applications, we aim to provide you with a nuanced understanding of the Low FODMAP Diet Chart.
Table of Contents
ToggleWhat are FODMAPs?
Have you ever heard the word FODMAPs and wondered what it means? Well, FODMAPs are not aliens or superheroes. They are actually types of foods that can sometimes make our tummies feel icky.
FODMAPs are special types of sugars and fibers found in things like fruits, veggies, grains, and even some sweeteners. When we eat foods with lots of FODMAPs, they can make our tummies feel bloated, gassy, or even give us a tummy ache.
To help our tummies feel better, some people follow a special diet called the low FODMAP diet. This means they try to eat less of those foods. By doing this, they can figure out which foods their tummies like and which ones they should avoid.
Remember, FODMAPs may be a big word, but understanding them can help us take better care of our tummies and feel happier and healthier overall!
Common High-FODMAP Foods
Have you ever wondered which foods might upset your tummy or cause discomfort? Well, some foods contain something called FODMAPs that can sometimes bother our tummies.
FODMAPs are special sugars and fibers found in certain foods. Here are some examples of high-FODMAP foods to be aware of:
Apples and pears: These fruits are yummy, but they contain high levels of FODMAPs. Try enjoying bananas or berries instead!
Milk and ice cream: Some dairy products can be high in FODMAPs, like regular cow’s milk and creamy ice cream. You can try lactose-free milk or dairy-free options like almond milk.
Wheat and rye: Foods made with wheat or rye, like bread and pasta, can be high in FODMAPs. You can look for gluten-free alternatives like rice or corn-based products.
Beans and lentils: While beans and lentils are packed with protein, they can also have lots of FODMAPs. Opt for low-FODMAP alternatives like tofu or lean meats.
How FODMAPs Affect Digestion
FODMAPs, which stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols, can have a significant impact on digestion, particularly for individuals with FODMAP sensitivity or conditions such as Irritable Bowel Syndrome (IBS). Here’s how FODMAPs affect digestion:
- Osmotic Effect: FODMAPs have an osmotic effect, which means they draw water into the intestines. This increased water content can lead to symptoms such as diarrhea and loose stools.
- Fermentation: FODMAPs are easily fermented by gut bacteria in the large intestine. During the fermentation process, gases like hydrogen, methane, and carbon dioxide are produced. Excessive gas can cause bloating, abdominal distension, and flatulence.
- Distension of the Bowel: The fermentation and gas production from FODMAPs can lead to the distension or stretching of the bowel. This can result in feelings of bloating, discomfort, and pain in the abdominal area.
- Increased Bowel Contractions: FODMAPs can stimulate increased bowel contractions or motility. This heightened activity can contribute to symptoms like cramping, urgency, and changes in bowel habits.
Benefits of the Low FODMAP Diet chart
The Low FODMAP diet chart offers several benefits for individuals with certain digestive issues, such as irritable bowel syndrome (IBS) or other functional gastrointestinal disorders. Here are some key benefits of the Low FODMAP diet:
Reduced tummy troubles: The low FODMAP diet chart helps us avoid foods that can make our tummies feel bloated, gassy, or have tummy aches. By eating FODMAP foods we can reduce these uncomfortable feelings.
Identifying trigger foods: The diet chart allows us to figure out which specific foods bother our tummies. By keeping a food diary and following the chart, we can learn which foods to avoid or eat less of in the future.
Improved digestion: When we eat foods low in FODMAPs, our digestive system can work better. This means less tummy troubles and more comfortable digestion overall.
Better energy levels: When our tummies feel good, we have more energy to do things we love, like running, playing, or learning new things. Following the low FODMAP diet can help us feel more energetic throughout the day.
Step-by-Step Guide to the Low FODMAP Diet
The low FODMAP diet is a complex dietary approach that involves several phases and careful attention to food choices. Here is a step-by-step guide to help you navigate the low FODMAP diet effectively:
- Educate Yourself: Start by familiarizing yourself with the concept of FODMAPs and their potential impact on digestive health. Understand the types of foods that are high and low in FODMAPs to make informed decisions during the diet.
- Consult with a Healthcare Professional: Before starting the low FODMAP diet, it’s essential to consult with a healthcare professional or a registered dietitian who specializes in the low FODMAP diet. They will assess your individual needs, provide guidance, and monitor your progress throughout the process.
- Elimination Phase: The elimination phase involves temporarily eliminating high-FODMAP foods from your diet. This phase typically lasts 2-6 weeks. During this time, you will avoid or limit foods such as onions, garlic, wheat, certain fruits, and dairy products that contain lactose.
- Meal Planning and Preparation: Plan your meals carefully during the elimination phase to ensure you’re still getting a balanced diet. Focus on low-FODMAP foods such as rice, potatoes, carrots, spinach, strawberries, and lactose-free dairy alternatives. Experiment with new recipes and explore low-FODMAP alternatives for your favorite dishes.
- Symptom Monitoring: Keep a food and symptom diary to track your progress and identify any potential triggers or improvements. Note down the foods you eat and any symptoms you experience. This information will help you and your dietitian make necessary adjustments during the reintroduction phase.
Potential Challenges and Considerations
While the low FODMAP diet can be effective in managing symptoms for individuals with FODMAP sensitivity or Irritable Bowel Syndrome (IBS), it also comes with potential challenges and considerations. Here are some factors to keep in mind:
- Dietary Restriction: The low FODMAP diet involves the temporary elimination of high-FODMAP foods, which can lead to a restricted food choices. This restriction may require careful meal planning and creativity in finding alternative ingredients and recipes to ensure a balanced and enjoyable diet.
- Nutritional Adequacy: Eliminating certain high-FODMAP foods can impact the intake of certain nutrients, such as fiber, prebiotics, and vitamins. It’s important to work with a registered dietitian to ensure nutritional adequacy during the elimination and reintroduction phases. They can provide guidance on suitable substitutions and the use of supplements if necessary.
- Reintroduction Challenges: The reintroduction phase can be complex and requires careful monitoring of symptoms. It can be challenging to determine individual tolerance levels for different FODMAP groups. Working closely with a dietitian during this phase is crucial to ensure accurate interpretation of symptoms and guidance on the appropriate progression of food reintroduction.
- Hidden FODMAPs: FODMAPs can be present in unexpected food sources, including processed foods, sauces, and condiments. Reading food labels carefully and being aware of potential hidden sources of FODMAPs is important to avoid inadvertently consuming high-FODMAP foods.
- Individual Variability: Every individual’s response to FODMAPs is unique. While some may have sensitivities to specific FODMAP groups, others may tolerate them well. It’s essential to recognize that the low FODMAP diet is not a one-size-fits-all approach. Personalized guidance from a registered dietitian can help navigate this variability and tailor the diet to individual needs.
Creating a Low FODMAP Diet Chart
Creating a Low FODMAP Diet Chart step by step involves a systematic approach to help you manage digestive discomfort. Here’s a comprehensive guide:
- Consult a Healthcare Professional: Before beginning a Low FODMAP Diet, consult with a healthcare professional, preferably a registered dietitian. They can assess your specific dietary needs and provide personalized guidance.
- FODMAP Education: Learn about FODMAPs, which are fermentable carbohydrates that can trigger digestive symptoms. Familiarize yourself with the four main categories: Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
- Food Diary: Keep a food diary for a week or more before starting the diet. Record all the foods and beverages you consume, as well as any digestive symptoms you experience. This will help identify potential trigger foods.
- Elimination Phase:
- Start with a strict elimination phase, during which you’ll avoid all high-FODMAP foods.
- This phase lasts 2-6 weeks, depending on your symptoms and healthcare provider’s recommendations.
- Focus on foods that are low in FODMAPs. Some examples include:
- Proteins: Chicken, turkey, fish, tofu, and eggs.
- Grains: Rice, quinoa, and gluten-free oats.
- Vegetables: Carrots, spinach, zucchini, and potatoes (without skin).
- Fruits: Bananas, blueberries, strawberries, and oranges (in limited quantities).
- Meal Planning:
- Plan your meals and snacks with low-FODMAP foods.
- Experiment with different recipes to keep your meals interesting and nutritious.
- Label Reading: When purchasing packaged foods, carefully read labels to identify high-FODMAP ingredients. Avoid items with high-FODMAP components like fructose, honey, and high-fructose corn syrup.
- Portion Control: Pay attention to portion sizes, as excessive consumption of low-FODMAP foods can increase FODMAP intake. For example, too many berries can become a high-FODMAP food.
- Symptom Monitoring: Continuously monitor your symptoms during the elimination phase. Note any changes in digestive discomfort and discuss them with your healthcare provider.
- Reintroduction Phase: After the elimination phase, start the reintroduction phase under the guidance of a dietitian. Gradually reintroduce one high-FODMAP food at a time, observing your body’s response.
- Customized Diet Plan: Work with your dietitian to create a personalized Low FODMAP Diet Chart that includes the foods you tolerate well and avoids those that trigger symptoms.
- Balanced Diet: Ensure your diet remains balanced and nutritious by incorporating a variety of low-FODMAP foods, including proteins, carbohydrates, fats, and a range of vitamins and minerals.
- Regular Monitoring: Continue to monitor your symptoms as you reintroduce foods and make adjustments to your diet.
- Meal Preparation: Plan and prepare your meals using low-FODMAP ingredients to have suitable options readily available.
- Long-Term Strategy: Remember that the Low FODMAP Diet is a diagnostic tool, not a permanent diet. It’s essential to work with your healthcare provider to develop a long-term dietary strategy that suits your needs.
Who Should Consider a Low FODMAP Diet
A Low FODMAP Diet is primarily considered for individuals who experience digestive issues, especially those with irritable bowel syndrome (IBS). Here are some groups of people who should consider this diet:
- IBS Patients: The Low FODMAP Diet is most recommended for individuals diagnosed with IBS, as it has been shown to help manage the symptoms of this condition.
- Functional Gut Disorders: People with other functional gut disorders, such as functional bloating or functional diarrhea, may also benefit from this diet.
- Digestive Discomfort: If you frequently experience symptoms like bloating, gas, abdominal pain, diarrhea, or constipation, even without an IBS diagnosis, a Low FODMAP Diet might help identify and alleviate trigger foods.
- Gluten Sensitivity: Some individuals who have been diagnosed with non-celiac gluten sensitivity may find relief from digestive symptoms by following a Low FODMAP Diet. It’s essential to differentiate between the two conditions.
- Inflammatory Bowel Disease (IBD): While a Low FODMAP Diet is not a primary treatment for Crohn’s disease or ulcerative colitis, some people with IBD find it helpful during periods of symptom flare-ups or as part of a broader dietary approach.
- Food Allergies and Intolerances: People with known food allergies or intolerances, such as lactose or fructose intolerance, can use this diet to help manage their symptoms.
- Athletes and Fitness Enthusiasts: Athletes and fitness enthusiasts may consider a Low FODMAP Diet to reduce gastrointestinal discomfort during training and competition, as intense exercise can sometimes trigger gut symptoms.
- Those Seeking Dietary Optimization: Some individuals without specific digestive disorders may also explore this diet to optimize their diet, reduce bloating, and improve their well-being.
Potential Challenges and How to Overcome Them
Embarking on a Low FODMAP Diet can present some challenges, but with proper planning and support, you can overcome them. Here are potential challenges and strategies to address them:
Limited Food Choices
Solution: Explore and familiarize yourself with low-FODMAP foods. There is a wide variety available, so focus on what you can eat rather than what you can’t.
Social Situations
Solution: Communicate your dietary needs to friends and family, and consider bringing your own low-FODMAP options to social gatherings. Educate your loved ones about your diet so they can provide support.
Traveling
Solution: Plan your meals and snacks in advance, and research low-FODMAP options at your travel destination. Consider carrying portable, non-perishable low-FODMAP foods when traveling.
Label Reading
Solution: Become proficient at reading food labels to identify high-FODMAP ingredients. Smartphone apps and websites that list low-FODMAP products can be helpful.
Dining Out
Solution: Check the menu in advance or call the restaurant to discuss your dietary needs. Many restaurants can accommodate special diets if they are informed ahead of time.
Nutritional Balance
Solution: Work with a registered dietitian to ensure you are getting all the necessary nutrients while on the diet. They can help you create balanced meal plans.
Boredom or Monotony
Solution: Experiment with new recipes and ingredients to keep your meals interesting. There are many creative low-FODMAP recipes available online and in cookbooks.
Stress and Mental Health
Solution: Stress can exacerbate digestive symptoms. Practice stress-reduction techniques such as yoga, meditation, or deep breathing exercises. Seek support from a therapist if needed.
Food Preparation
Solution: Preparing low-FODMAP meals may require some adjustments to your usual cooking routines. Invest in kitchen gadgets and tools that make meal preparation easier.
Conclusion
Low FODMAP Diet Chart is a valuable resource for individuals seeking relief from digestive discomfort, particularly those with conditions like irritable bowel syndrome (IBS).
By carefully selecting and planning meals based on low-FODMAP foods, individuals can significantly reduce symptoms such as bloating, gas, and abdominal pain, ultimately improving their quality of life.
It’s important to emphasize that this diet should be undertaken with the guidance of healthcare professionals or registered dietitians.The diet’s strength lies in its customization, enabling each person to create a personalized plan that suits their unique dietary needs and identifies specific trigger foods.
The journey through the Low FODMAP Diet may present challenges, from limited food choices to social and emotional aspects.
However, with proper education, support, and a focus on what can be enjoyed rather than what must be avoided, these obstacles can be overcome.
Ultimately, the Low FODMAP Diet Chart serves as a valuable tool in the journey towards better digestive health, helping individuals discover which foods work best for their bodies and enabling them to make informed dietary choices that contribute to their well-being.
FAQs
Of course, here are some frequently asked questions (FAQs) related to the Low FODMAP Diet Chart:
What is a Low FODMAP Diet Chart?
A Low FODMAP Diet Chart is a dietary plan that helps manage digestive discomfort, particularly for those with conditions like irritable bowel syndrome (IBS). It focuses on foods low in fermentable carbohydrates called FODMAPs.
Who should consider following a Low FODMAP Diet Chart?
This diet is recommended for individuals with IBS, functional gut disorders, and those with food intolerances. It can also be considered by people seeking relief from digestive symptoms such as bloating and gas.
What are FODMAPs?
FODMAPs are fermentable oligosaccharides, disaccharides, monosaccharides, and polyols—specific types of carbohydrates found in various foods. They can trigger gastrointestinal symptoms in some individuals.
How long should I follow a Low FODMAP Diet?
A Low FODMAP Diet is divided into an elimination phase (2-6 weeks) and a reintroduction phase (2-8 weeks). The goal is to identify trigger foods and then return to a more balanced diet while avoiding only the specific FODMAPs that affect you.
What foods are typically high in FODMAPs?
High-FODMAP foods include certain fruits (e.g., apples, pears), vegetables (e.g., onions, garlic), grains (e.g., wheat), and dairy products (e.g., milk, yogurt).
What foods are typically low in FODMAPs?
Low-FODMAP foods include meats, fish, eggs, rice, quinoa, carrots, spinach, bananas, and many more. There is a wide variety of low-FODMAP options.
Is a Low FODMAP Diet permanent?
No, it’s not meant to be a permanent diet. Its purpose is to identify trigger foods. After the elimination and reintroduction phases, you can return to a more balanced diet while avoiding only specific high-FODMAP foods that affect you.